 |
| Chart by Hannah Recht, Kaiser Health News |
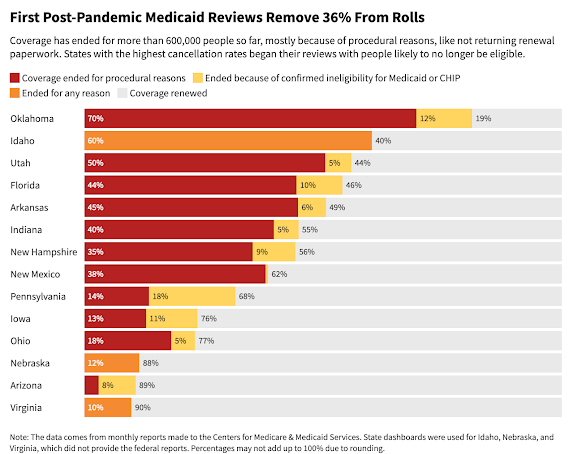
As Medicaid "unwinds" from pandemic levels, millions of Americans have lost health care coverage primarily because of paperwork issues, not a lack of eligibility, reports Hannah Recht of KFF Health News. "Four out of every five people dropped so far either never returned the paperwork or omitted required documents, according to a KHN analysis of data from 11 states that provided details on recent cancellations. . . . Before the unwinding, more than 1 in 4 Americans — 93 million — were covered by Medicaid or the Children's Health Insurance Program, according to KFF Health News' analysis of the latest enrollment data."
Each state has its own review process schedule, which creates vast differences in who and when people lose coverage. "Nearly 56% of people included in early reviews were dropped in Utah. In New Hampshire, 44% received cancellation letters within the first two months — almost all for procedural reasons, like not returning paperwork," Rechet reports. "Because of the three-year pause in renewals, many people on Medicaid have never been through the process or aren't aware they may need to fill out long verification forms, as a recent KFF poll found. Some people moved and didn't update their contact information."
Half of U.S. children are insured by Medicaid or CHIP. "Tens of thousands of children are losing coverage, as researchers have warned, even though some may still qualify," Recht reports. "In its first month of reviews, South Dakota ended coverage for 10% of all Medicaid and CHIP enrollees in the state. More than half of them were children. In Arkansas, about 40% were kids. . . . Many parents don't know that limits on household income are significantly higher for children than adults. Parents should fill out renewal forms even if they don't qualify themselves, said Joan Alker, executive director of the Georgetown University Center for Children and Families."
Some states have opted to review families with children at the "end of the review process," giving parents more time to fulfill eligibility requirements. Recht reports: "Advocacy coalitions in both Florida and Arkansas also have called for investigations into the review process and a pause on cancellations. . . . Federal law requires states to tell people why they're losing Medicaid coverage and how to appeal the decision. . . . . Indiana State Rep. Ed Clere (R) pushed his state's Medicaid officials to immediately make changes to avoid people unnecessarily becoming uninsured. One official responded that they'd learn and improve over time. Clere replied he'd rather not 'learn. . . at their expense.'"

No comments:
Post a Comment